What Are Familial Breast And Ovarian Cancer? Are You At Risk?
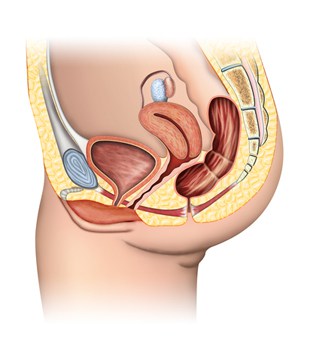
Family members can share many traits such as red hair, straight teeth, or an outgoing personality. Unfortunately, they can also share traits linked to specific diseases. Approximately 5%-10% of all breast and ovarian cancer cases are hereditary, meaning two first-degree (mother, daughter, or sister) or second-degree (grandmother or aunt) blood relatives shared this disease. Both breast and ovarian cancer are characterized by the uncontrollable growth of abnormal cells. If these abnormal cells are not removed, they can keep reproducing to form a larger mass and eventually spread to other tissues of the body.
Given that family members share genetic material, i.e. DNA, research has linked approximately half of these cancer cases to a shared mutation in the DNA that encodes the BRCA1 and/or BRCA2 genes. The BRCA1/2 genes produce proteins whose function is to repair damaged pieces of DNA. Multiple mutations throughout these gene regions are linked to an increased risk of developing breast and ovarian cancers. While the likelihood of a person in the general population developing breast or ovarian cancer by age 70 is approximately 12% and 1%, respectively, a person exhibiting a BRCA1/2 gene mutation has a 50% chance of developing breast cancer and 25% chance of developing ovarian cancer by 70.
People with these hereditary mutations may also develop breast and ovarian cancer at an earlier age than people in the general population. Furthermore, while breast cancer is primarily thought of as affecting mainly women, BRCA1/2 mutations also increase the chances of men developing breast cancer to approximately 5% by age 70. Men can also pass on the mutated form of these genes to their offspring.
Who Should Be Tested For BRCA1/2 Mutations?
Individuals who are serious about genetic testing are advised to receive counseling by a genetic counselor before and after testing. While there are no standard testing criteria, Europe’s Society for Medical Oncology (ESMO) and the United States National Cancer Institute (NCI) suggest the following people should receive genetic tests for mutations in the BRCA1 and BRCA2 genes:
- any relative with a harmful BRCA1 or BRCA2 mutation
- two first-degree relatives (mother, daughter, or sister) are diagnosed with breast cancer, one of whom was diagnosed at age 50 or younger
- three or more first-degree or second-degree (grandmother or aunt) relatives are diagnosed with breast cancer
- a combination of first- and second-degree relatives are diagnosed with breast cancer and ovarian cancer (one cancer type per person)
- a first-degree relative is diagnosed with cancer in both breasts (bilateral breast cancer)
- a combination of two or more first- or second-degree relatives are diagnosed with ovarian cancer
- a first- or second-degree relative is diagnosed with both breast and ovarian cancer
- breast cancer is diagnosed in a male relative
Furthermore, people of Ashkenazi Jewish descent exhibit an especially high familial increased cancer risk and should receive BRCA1/2 testing if:
- any first-degree relative is diagnosed with breast or ovarian cancer
- two second-degree relatives on the same side of the family are diagnosed with breast or ovarian cancer
Though the frequency of BRCA1/2 mutations in the general population is rare, anyone concerned about their personal cancer risks can be tested to know their genetic status (National Cancer Institute).
Should You Undertake Genetic Testing?
Though the prospect of discovering an increased risk for cancer can be terrifying, the good news is there are preventative measures you can take to delay your risk and identify cancer early in the process. The earlier the discovery, the better the chance of a longer and healthier life. Testing will also allow you to give your family insight into their own genetic health, so that they can make informed decisions about their health.
How Can You Take Action If You Have BRCA1/2 Mutations?
Even if your results determine you have a cancer associated mutation in the BRCA1/2 regions, this does not conclusively determine you will get breast or ovarian cancer. You can, however, take pre-emptive measures to delay or preclude your chances of breast and ovarian cancer.
Simple initial steps are to get enough daily exercise, maintain a healthy weight, and reduce or abstain from alcohol usage, all of which are associated with a delay in cancer occurrence and a better outcome if cancer develops. Frequent self-examinations of the breast and mammograms starting at an early age may identify potential problems that can be resolved before breast cancer develops. For ovarian cancer, monitoring levels of the protein CA125 from an early age may aid in prevention.
More intensive preventative measures can include surgical intervention whereby the breast and ovary tissue are removed prior to cancer development. Chemotherapeutic drugs can also be taken before cancer develops to reduce the risk of occurrence. While these methods have proven effective, they can have serious physical and emotional consequences and should be discussed with medical doctors and family members before being applied.
References
- Balmaña J, Díez O, Castiglione M; ESMO Guidelines Working Group. BRCA in breast cancer: ESMO clinical recommendations. Ann Oncol. 2009;20 Suppl 4:19-20.
- Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25:1329-33.
- Ferla R, Calò V, Cascio S, et al. Founder mutations in BRCA1 and BRCA2 genes. Ann Oncol. 2007;18 Suppl 6:vi93-8.
- King MC, Marks JH, Mandell JB; New York Breast Cancer Study Group. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science. 2003;302:643-6.
- National Cancer Institute. BRCA1 and BRCA2: Cancer Risk and Genetic Testing. Available at: <href=”#r15″>http://www.cancer.gov/cancertopics/factsheet/Risk/BRCA#r15. Accessibility verified October 8, 2012
Last Reviewed: 27-Jan-2014